Item 25/100: Cancer Fighting…Bacteria
James Budnick, PhD, Senior Scientist
ATCC® BAA-3199™ – Salmonella enterica subsp. enterica (Kauffmann and Edwards) Le Minor and Popoff
In 1891, a bone sarcoma surgeon injected a cancer patient with streptococcal bacteria in the hope that it would induce an immune response large enough to cause the cancer to regress.1 That surgeon was William Coley and he was successful. This led to his creation of “Coley’s Toxins,” a mixture of Streptococcus pyogenes and Serratia marcescens that he used to treat cancer patients. This important work would lay the foundation for future cancer immunotherapy research, earning Coley the title “Father of Immunotherapy.”2 Later on in 1935, George Shwartzman would observe the antitumor therapeutic effects of Salmonella (formerly Bacillus typhosus) in mice.3 While these therapies showed success and promise, they were highly scrutinized and concerns arose over the ethics of injecting patients with pathogens. The development of radiation and chemotherapy eventually led to the decreased use of these therapeutics.
However, as science advanced, the antitumor effects of microbes came under the spotlight again. Salmonella in particular has been studied for not only its ability to stimulate an immune response, kill tumor cells, and improve tumor recognition by the host but also for its function as a potential vehicle for drug delivery as bacteria have been shown to directly colonize tumor tissues.2 This led to the engineering and patenting of a tumor-targeting strain of Salmonella—Salmonella enterica serovar Typhimurium 14028S, VNP20009 (YS1646, cited in US Pat. No. 6,447,784 as 202165).4,5 This strain has been used throughout the scientific community to study tumor inhibition by the bacterium (PubMed). Currently, an ATCC-manufactured and accessioned progeny of this strain is available from ATCC as Salmonella enterica subsp. enterica strain YS1646 (ATCC® BAA-3199™).
Salmonella is not the only organism that has been studied for its tumor targeting capabilities. Clostridium, Listeria, Bifidobacterium, Escherichia, Caulobacter, and Proteus species have also been examined as anticancer therapeutics.6-8 What is surprising is the fact that these are highly pathogenic organisms, so the key is to engineer an effective but also safe (less virulent) organism to use as a therapeutic. Studies have pointed out that while many engineered bacterial cancer therapies are promising, the heterogeneity of cancers makes it difficult to produce single agent cure and that these organisms can instead be synergistic in their effectiveness with other therapies.6
Item 26/100: Immune Cells with Therapeutic Potential
Meghan Sikes, MS, Senior Biologist
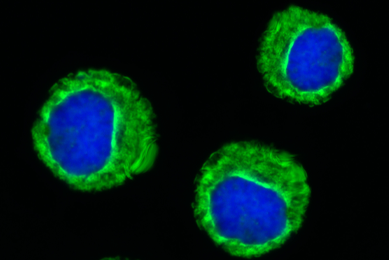
ATCC® PCS-800-017™ – Primary CD8+ Cytotoxic T Cells
Our T lymphocytes act as security guards, patrolling our body for foreign materials and pathogens to keep us healthy from various diseases. Originating from stem cells in bone marrow, there are two main classes of T cells in the human adaptive immune system: CD4+ and CD8+ T cells. CD8+ cytotoxic T cells interact with major histocompatibility complex class-1 molecules on cell surfaces to kill infected cells or tumor cells.
Due to CD8+ T cells functionality, they have become a revolutionary player in cancer immunotherapy as CAR-T cells.9 Using a viral vector, CD8+ T cells can be transduced to express chimeric antigen receptors (CAR’s) that recognize specific cancer cells and tumors. Despite some hurdles, CAR-T cells have shown success in blood cancer treatments and have recently showed promise against solid tumors.10
CD8+ T cells have many applications in cancer and immunotherapy research. For instance, the presence of CD8+ T cells are associated with favorable outcomes in breast cancer patients and T cell densities in tumors can be used in clinical outcome predictions.11 Additionally, CD8+ cytotoxic T cells have been shown to have higher infiltration of colorectal tumor microenvironments than CD4+ T cells, and they produce signaling molecules such as IL-2 and IFN-γ to enhance cytotoxic potential.12 Overall, CD8+ cytotoxic T cells are essential components of cancer and infectious disease control and are promising immunotherapeutic agents.13
Item 27/100: Opportunistic Infections – The Tooth be Told
Sydney McKnight, MS, Biologist
ATCC® 51191™ – Fusobacterium nucleatum subsp. animalis Gharbia and Shah
Fusobacterium nucleatum is a non-motile, gram-negative anaerobe that is typically found in the oral cavity.14 While this bacterial species is primarily known as a periodontal pathogen, it has been recently linked to the development of colorectal cancer—the second leading cause of cancer-related deaths in the United States.15-17 F. nucleatum can translocate from the mouth to the gut either through the bloodstream or via the digestive tract, often during activities such as chewing or dental procedures.18,19 Once in the colorectal environment, F. nucleatum promotes tumor development by inducing inflammation and manipulating the host's immune response.20
This opportunistic bacterium binds to host cells and other microorganisms through its adhesion factors, facilitating its survival and proliferation within the gut microbiota. A high concentration of F. nucleatum in colorectal tissues have been associated with poorer patient outcomes, including increased rates of cancer recurrence and resistance to chemotherapy.21 F. nucleatum subsp. animalis (ATCC® 51191™) has played a pivotal role in exploring how the bacterium interacts with host cells and contributes to tumorigenesis, aiding in the identification of potential therapeutic strategies to combat CRC.16,21-23 As research progresses, F. nucleatum has been increasingly highlighted as not only a mutualistic organism, but also as a significant opportunist in cancer biology, reinforcing the need for integrated approaches to health that consider the interplay between oral and gastrointestinal microbiomes.
Item 28/100: Elevating Industry Standards with CAR-T Target Reporter Cell Lines
Hyeyoun Chang, PhD, Senior Scientist
ATCC® CRL-3580-GFP-LUC2™ – NCI-H929-GFP-Luc2
Chimeric antigen receptor (CAR)-T cell therapy is a type of cancer immunotherapy that utilizes patient’s own T cells. Taken from a patient’s blood, T cells are genetically modified to express CAR that binds to a specific antigen on the surface of cancer cells for cancer cell killing. CAR-T cell therapy has shown remarkable efficacy, higher durability than conventional chemotherapy, and expandability beyond B-cell hematological malignancies. Its clinical success has marked a significant advancement in personalized cancer treatment.24
Development of CAR-T therapy involves evaluating the functionality of CAR-T cells ex vivo. However, there are various limitations to the currently available standalone CAR-T cell–mediated cytotoxicity assays.25 At ATCC, we generated a panel of luciferase reporter and GFP-luciferase double reporter cell lines that endogenously express high levels of clinically relevant CAR-T target antigens, such as CD19, CD20, Her2, and BCMA. These CAR-T target reporter cell lines enable combination of bioluminescence assays with phase contrast and fluorescence live cell imaging for enhanced sensitivity and higher spatial and temporal resolution compared to the traditional methods. This multimodal approach allows us to overcome the limitations associated with individual assay methods while improving overall assay performance.26
Item 29/100: Examining Burkitt’s Lymphoma Through Reporter Cancer Cell Lines
Kenneth Montenegro, AS, Associate Biologist Intern (SPARC Program)
ATCC® CCL-86-Luc2™ – Raji-Luc2
The rare disease known as Burkitt’s Lymphoma is attributed to the proliferation of irregular, mature B Lymphocytes in the human tissue. Cellular characteristics of the malignancy include cytoplasmic vacuolization and high levels of CD19 expressed endogenously. Although treatment is dependent on the age of the patient and stage, it may prove difficult at times due to the disease’s association with Epstein-Barr Virus and Human Immunodeficiency Virus.27 To better understand underlying components of the disease, reporter cancer cell models can be used for its examination in an in vitro setting. The stable expression and reliability of reporter genes serves as a remarkable opportunity for its utilization in immunological and cancer research applications.
Using Raji (ATCC® CCL-86™) as the parental cell line, we developed the Raji-Luc2 reporter cell line (ATCC® CCL-86-Luc2™) via transduction with a lentiviral vector encoding the firefly luciferase gene (luc2) under the control of the EF-1 alpha promoter. The introduction of this gene has allowed researchers to develop assays in measuring cell viability and cytotoxicity using a Burkitt’s Lymphoma model. With CD19 being identified as only one of two FDA-approved CAR-T targets, luciferase expression in Raji-Luc2 can be used to quantify CAR-T killing of B lymphocytes through luminescence.27 Not only does this highlight the significance of using reporter cell lines, but it also provides clinical information on the efficacy of treatments options such as CAR-T cell therapy in cancer patients.
It is important to note that advancements in science are only made possible through the collaboration between different scientific fields. The example of using a subclass of retroviruses for gene delivery in cancer cells demonstrates this in great fashion. The continuation of these discoveries will create pathways towards a wider range of treatment options and possible cures in human malignancies.
Item 30/100: Colon Cancer on the Rise in Younger Populations
Meghan Sikes, MS, Senior Biologist
ATCC® CCL-222™ – COLO 205
If you are over the age of 45, you’ve most likely been recommended by your doctor to have a colonoscopy for colon cancer screening. Colorectal cancers are the second leading cause of cancer-related mortality worldwide, and concerningly, incidence rates in young people are increasing.28 The rising rates in young people are not fully understood, but researchers suspect that environment, diet, genetic background, and even microplastics play a role.29 Colorectal cancer growth begins in the epithelial cells of the colon or the rectum, and typically develop in the lining of the large intestine, forming precancerous polyps. Adenocarcinomas are by far the most common type of colorectal cancer, responsible for up to 95% of all cases.30
ATCC supports research on this type of cancer by providing highly authenticated colon adenocarcinoma cell lines. COLO 205 (ATCC® CCL-222™) is an adenocarcinoma tumor cell line that was isolated in 1975 from abdominal fluid in a male patient with colon adenocarcinoma.31 This colon cancer cell line is tumorigenic in mice and serves as a useful research tool for colon cancer research, which may lead to finding more effective treatment options.
Item 31/100: The SK-BR-3 Cell Line Enabled a Milestone in Cancer Research History
Fang Tian, PhD, Director Cell Biology Content and Product Development
ATCC® HTB-30™ – SK-BR-3 [SKBR3]
Breast cancer is one of the leading causes of cancer-related death in women in the United States, second only to lung cancer. In 1984, researchers discover the new oncogene HER2 (ErbB2), which is overexpressed in about 20% to 25% of breast cancer and is associated with more aggressive disease and a poor prognosis. In 1998, the first monoclonal antibody against an oncogene was approved by FDA.32 This monoclonal antibody drug, called trastuzumab (herceptin), specifically targets cancer cells that overexpress the HER2 gene, enabling the treatment of women with HER2-positive metastatic breast cancer. This single drug changed our entire approach to cancer therapy. The story behind this milestone in cancer research and therapy33 is fascinating, and a particular cell line from ATCC played a critical role.
Established in 1970 from the pleural effusion of a 43-year-old Caucasian female with malignant adenocarcinoma of the breast, SK-BR-3 (ATCC® HTB-30™) is a human breast cancer cell line that overexpresses HER2. This cell line became a vital tool as it closely models HER2-positive breast cancer. Dr. Alex Ullrich’s team at Genentech used SK-BR-3 and other cancer cell lines obtained from ATCC to characterize a HER2-targeted therapeutic antibody.34 Genentech continued to develop the antibody as trastuzumab (herceptin) and received FDA approval for the treatment of HER2-positive metastatic breast cancer in 1998.35 Today, HER2-positive breast cancer patients worldwide have benefited immensely from the innovation of HER2-directed therapeutics. SK-BR-3 continues representing the most widely studied breast cancer cell lines, with applications ranging from basic cancer research to preclinical studies for anti-cancer therapeutics. Impressively, our understanding and characterization of this classic breast cancer cell line is still evolving.36
Item 32/100: Epithelial-Mesenchymal Transition Reporter Cells
Diana Douglas, BS, Lead Biologist
ATCC® CCL-185EMT™ – A-549 VIM RFP
Lung cancer is the third most prevalent cancer type in the United States. It contributes to more cancer-related mortalities than any form of cancer. This is due, in part, to the fact that most lung cancers are found after the cancer has metastasized to other parts of the body.37 Scientists need dynamic models and technologies to further their research and understanding of cancer and metastasis and make improvements in treatment options. Epithelial-mesenchymal transition (EMT) and its reverse program, mesenchymal-epithelial transition (MET), are developmental programs that have been shown to play critical roles in promoting metastasis in carcinoma. As cells shift from epithelial to mesenchymal, they lose epithelial characteristics, including apicobasal polarity and cell-cell adhesions, and they gain front back polarity and cell matrix interactions, which allow them to migrate and invade.38 Re-activation of MET has been implicated in the establishment of distal metastasis.39 Cells can transition between EMT and MET, and a number of intermediate states, as cancer progresses.
A-549 VIM RFP (ATCC® CCL-185EMT™) was created at ATCC using the CRISPR/Cas9 gene-editing platform and the parental A549 (ATCC® CCL-185™) non-small cell lung cancer (NSCLC) cell line (a standard for studying EMT in cancer metastasis within the lung cancer research community). This reporter cell line is designed to enable the real-time monitoring of the changing status of cells from epithelial to mesenchymal via the expression of red fluorescent protein (RFP)-tagged vimentin. Functional evaluation of A-549 VIM RFP shows sensitivity to anti-EMT drugs PP1 and A83-1. This provides the foundation for the high-throughput (HTS) identification of new anti-EMT drugs for metastatic NSCLC therapy. The A-549 VIM RFP reporter cell line provides a visualizable, convenient, and sensitive platform for research on the mechanisms of metastasis in vitro and the development of new antitumor drugs for metastatic NSCLC. ATCC has a portfolio of EMT/EMT reporter cell lines that were generated using prevalent cancer cell lines. These tools can aid scientists in achieving a better understanding the mechanistic and clinical implications of EMT, ultimately translating into a better understanding of and improved treatments for cancer.
Item 33/100: Enhanced Workflow of Cancer Immunotherapy Drug Discovery Through Immune Checkpoint Reporter Cell Lines
Hyeyoun Chang, PhD, Senior Scientist
ATCC® CRL-1942-NFAT-LUC2™ – SUP-T1 NFAT-Luc2
Cancer immunotherapy is a type of cancer treatment that utilizes the patient’s own immune system to fight cancer. Although the human immune system works very effectively to detect and protect the body from abnormal cells that can become cancerous, cancer is a complicated disease that can bypass and outsmart the immune system. One of the ways that cancer cells avoid immune detection is through overexpressing immune checkpoint proteins on the cell surface. Immune checkpoints are a normal part of the immune system that prevents T cells from becoming too strong and damaging healthy cells by acting like a “brake” when bound to their partner proteins. Some cancer cells take advantage of this system and stealthily grow without being eliminated by the immune cells. A class of immunotherapy drugs called immune checkpoint inhibitors works by blocking immune checkpoint proteins from binding their partners. This exposes cancer cells to immune surveillance that leads to cancer cell death. Immune checkpoint therapy rapidly became successful and has become the standard of care in many different cancer types. The discovery and development of novel immune checkpoint inhibitors, however, is challenged by the intrinsic complexity of the immunological models. To provide with a solution, ATCC has developed immune checkpoint reporter cell lines that endogenously express high levels of immune checkpoint proteins. These cancer cell lines, T cell lines, myeloid cell lines, and B cell line report early-stage immune activation by expressing luciferase enzyme that can be easily detected and quantified to evaluate the efficacy, potency, and dynamics of the immune checkpoint inhibitor.40
Item 34/100: Cervical Cancer Cells to Improve Global Outcomes
Meghan Sikes, MS, Senior Biologist
ATCC® HTB-35™ – SiHa
In 2006, the FDA approved a groundbreaking quadrivalent vaccine for administration around ages 11-12 that was aimed to prevent four types of human papillomavirus (HPV).41 This vaccine was monumental at the time as the goal was to prevent cervical cancer, which is the fourth most common cancer in women globally and is caused by oncogenic HPV’s in 99.7% of cervical carcinoma cases.42 Amazingly, since the international introduction of the HPV vaccine in the mid-2000’s, the risk of cervical cancer in vaccinated women is lower as compared to unvaccinated women.43
Despite the pivotal vaccine helping to reduce cervical cancer rates, there are still research areas to be explored to try to reach better global cervical cancer control. For oncological studies, ATCC’s SiHa cell line (ATCC® HTB-35™) provides a solution with applications such as cancer research and sexually transmitted disease research. The SiHa cell line was established in 1970 from the tissue sample of 55-year-old Japanese patient with cervical carcinoma.44 Deposited with ATCC by Yohei Ito, SiHa cells have integrated HPV-16 DNA sequences46 and these sequences can trigger expression of the viral oncogenes E6 and E7, which can cause degradation of the tumor suppressor proteins p53 and pRb. 45
With the tumorigenic properties of SiHa cells, it’s no surprise that there are currently various research topics utilizing the cell line and contributing to cervical cancer research. For instance, recent research into cancer therapeutics with SiHa cells has suggested that an omega-3 fatty acid could epigenetically affect the growth of cervical cancer cell lines.46 Another study from 2023 showed that biosynthetic zinc oxide nanoparticles were cytotoxic against SiHa cells, indicating that nanoparticles could be leveraged in cancer treatment strategies.47 Continuing research on cervical cancers can help us to find better treatments and improve prognoses globally.
Did you know?
As of January 2022, there were an estimated 18.1 million cancer survivors in the United States. The number of cancer survivors is projected to increase to 22.5 million by 2032.42
Explore more resources
Oncology and Immuno-oncology
Support your oncology and immuno-oncology research with authenticated cell lines, patient-derived cancer models, human primary immune cells, and advanced cell models from ATCC.
More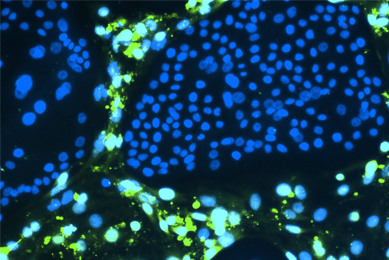
Human Cancer Models Initiative (HCMI)
ATCC is the exclusive distributor of the Human Cancer Models Initiative (HCMI) models. See the models that include common and rare examples of cancer from numerous tissues.
MoreThawReady™ Assay Ready Cells
ATCC's ThawReady™ Assay Ready Cells will streamline your workflows by months, allowing you to focus on advancing drug discovery and development.
MoreReferences
- McCarthy EF. The toxins of William B. Coley and the treatment of bone and soft-tissue sarcomas. Iowa Orthop J 26: 154-158, 2006. PubMed: 16789469
- Wang D, et al. Perspectives on Oncolytic Salmonella in Cancer Immunotherapy—A Promising Strategy. Front Immunol 12: 615930, 2021. PubMed: 33717106
- Shwartzman G. 1935. HEMORRHAGIC NECROSIS AND REGRESSION SARCOMA 180. Science 82(2122): 201, 1935. PubMed: 17844582
- Broadway KM, et al. Complete genome sequence of Salmonella enterica serovar Typhimurium VNP20009, a strain engineered for tumor targeting. J Biotechnol 192:177–178, 2014. PubMed: 5046822
- Bermedues D, Low KB. Genetically modified tumor-targeted bacteria with reduced virulence (U.S. Patent No. 6,447,784). U.S. Patent and Trademark Office, 2002. Available online: https://patents.google.com/patent/US6447784B1/en
- Zhou S, et al. Tumour-targeting bacteria engineered to fight cancer. Nat Rev Cancer 18(12): 727–743, 2018. PubMed: 30405213
- Faghfoori Z, et al. Anticancer effects of bifidobacteria on colon cancer cell lines. Cancer Cell Int 21(1): 258, 2021. PubMed: 33980239
- Forbes NS. Engineering the perfect (bacterial) cancer therapy. Nat Rev Cancer 10(11): 785–794, 2010. PubMed: 20944664
- Raskov H, et al. Cytotoxic CD8+ T cells in cancer and cancer immunotherapy. Br J Cancer 124(2): 359–367, 2021. PubMed: 32929195
- Huang H, et al. Advances in CAR-T cell therapy for hematologic and solid malignancies: latest updates from 2024 ESMO Congress. J Hematol Oncol 17(1): 120, 2024. PubMed: 39639359
- Fortis SP, et al. Differential intratumoral distributions of CD8 and CD163 immune cells as prognostic biomarkers in breast cancer. J Immunother Cancer 5: 39, 2017. PubMed: 28428887
- Yu B, et al. Immunotherapy for colorectal cancer. Front Immunol 15: 1433315, 2024. PubMed: 39238638
- Zhou Z, et al. Optimizing CD8+ T cell-based immunotherapy via metabolic interventions: a comprehensive review of intrinsic and extrinsic modulators. Exp Hematol Oncol 13(1): 103, 2024. PubMed: 39438986
- Muchova M, et al. Fusobacterium nucleatum elicits subspecies-specific responses in human neutrophils. Front Cell Infect Microbiol 14: 1449539, 2024. PubMed: 39450334
- American Cancer Society. (n.d.). What is colorectal cancer? In American Cancer Society [Report]. Available online: https://www.cancer.org/content/dam/CRC/PDF/Public/8604.00.pdf
- Rubinstein MR, et al. Fusobacterium nucleatum Promotes Colorectal Carcinogenesis by Modulating E-Cadherin/β-Catenin Signaling via its FadA Adhesin. Cell Host Microbe 14(2): 195–206, 2013. PubMed: 23954158
- Wu Z, et al. The Role of Fusobacterium nucleatum in Colorectal Cancer Cell Proliferation and Migration. Cancers (Basel) 14(21): 5350, 2022. PubMed: 36358769
- Abed J, et al. Colon Cancer-Associated Fusobacterium nucleatum May Originate From the Oral Cavity and Reach Colon Tumors via the Circulatory System.Front Cell Infect Microbiol 10: 400, 2020. PubMed: 32850497
- Pignatelli P, et al. The Role of Fusobacterium nucleatum in Oral and Colorectal Carcinogenesis. Microorganisms 11(9): 2358, 2023. PubMed: 37764202
- Wu J, Li Q, Fu X. Fusobacterium nucleatum Contributes to the Carcinogenesis of Colorectal Cancer by Inducing Inflammation and Suppressing Host Immunity. Transl Oncol 12(6): 846–851, 2019. PubMed: 30986689
- Lamprinaki D, et al. Siglec-7 Mediates Immunomodulation by Colorectal Cancer-Associated Fusobacterium nucleatum ssp. animalis. Front Immunol 12: 744184, 2021. PubMed: 34659241
- González A, et al. New Insights into Mucosa-Associated Microbiota in Paired Tumor and Non-Tumor Adjacent Mucosal Tissues in Colorectal Cancer Patients. Cancers (Basel) 16(23): 4008, 2024. PubMed: 39682194
- Zhang H, et al. Disease-associated gut microbiome and critical metabolomic alterations in patients with colorectal cancer. Cancer Med 12(14): 15720–15735, 2023. PubMed: 37260140
- Wang JY, Wang L. CAR-T cell therapy: Where are we now, and where are we heading?. Blood Sci 5(4): 237-248, 2023. PubMed: 37941917
- Swan D, Madduri D, Hocking J. CAR-T cell therapy in Multiple Myeloma: current status and future challenges. Blood Cancer J 14(1): 206, 2024. PubMed: 39592597
- Foulke JG, et al. Optimizing Ex Vivo CAR-T Cell-Mediated Cytotoxicity Assay through Multimodality Imaging. Cancers (Basel) 16(14): 2497, 2024. PubMed: 39061136
- Graham BS, Lynch DT. Burkitt Lymphoma. [Updated 2023 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available online: https://www.ncbi.nlm.nih.gov/books/NBK538148/
- Menon G, Cagir B. Colon Cancer. 2024 Dec 21. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan. PubMed: 29262132
- Chartres N, et al. Effects of Microplastic Exposure on Human Digestive, Reproductive, and Respiratory Health: A Rapid Systematic Review. Environ Sci Technol 58(52): 22843-22864, 2024. PubMed: 39692326
- City of Hope. Colorectal cancer types. Page updated August 11, 2022. Available online: https://www.cancercenter.com/cancer-types/colorectal-cancer/types.
- Semple TU, et al. Tumor and lymphoid cell lines from a patient with carcinoma of the colon for a cytotoxicity model. Cancer Res 38(5): 1345-1355, 1978. PubMed: 565251
- National Cancer Institute. Milestones in Cancer Research and Discovery. Page updated February 21, 2025. Available online: https://www.cancer.gov/research/progress/250-years-milestones
- Sawyers CL. Herceptin: A First Assault on Oncogenes that Launched a Revolution. Cell 179(1): 8–12, 2019. PubMed: 31519311
- Hudziak RM, et al. p185HER2 monoclonal antibody has antiproliferative effects in vitro and sensitizes human breast tumor cells to tumor necrosis factor. Mol Cell Biol 9(3): 1165–1172, 1989. PubMed: 2566907
- U.S. Food and Drug Administration. Drugs@FDA. Accessed August 18, 2017. Available online: https://www.accessdata.fda.gov/scripts/cder/daf/
- Nattestad M, et al. Complex rearrangements and oncogene amplifications revealed by long-read DNA and RNA sequencing of a breast cancer cell line. Genome Res 28(8): 1126–1135, 2018. PubMed: 29954844
- National Cancer Institute. Cancer statistics. Page updated May 9, 2024. Available online: https://www.cancer.gov/about-cancer/understanding/statistics
- Ribatti D, Tamma R, Annese T. Epithelial-Mesenchymal Transition in Cancer: A Historical Overview. Transl Oncol 13(6): 100773, 2020. PubMed: 32334405
- van Zijl F, Krupitza G, Mikulits W. Initial steps of metastasis: cell invasion and endothelial transmigration. Mutat Res 728(1-2): 23–34, 2011. PubMed: 21605699
- Chang H, et al. GAS-Luc2 Reporter Cell Lines for Immune Checkpoint Drug Screening in Solid Tumors. Cancers (Basel) 16(11): 1965, 2024. PubMed: 38893085
- McLemore MR. Gardasil: Introducing the new human papillomavirus vaccine. Clin J Oncol Nurs 10(5): 559-560, 2006. PubMed: 17063609
- Okunade KS. Human papillomavirus and cervical cancer. J Obstet Gynaecol 40(5): 602-608, 2020. PubMed: 31500479
- Lei J, et al. HPV Vaccination and the Risk of Invasive Cervical Cancer. N Engl J Med 383(14): 1340-1348, 2020. PubMed: 32997908
- Friedl F, Kimura I, Osato T, Ito Y. Studies on a new human cell line (SiHa) derived from carcinoma of uterus. I. Its establishment and morphology. Proc Soc Exp Biol Med 135(2): 543-545, 1970. PubMed: 5529598
- Yu L, et al. HPV oncogenes expressed from only one of multiple integrated HPV DNA copies drive clonal cell expansion in cervical cancer. mBio 15(5): e0072924, 2024. PubMed: 38624210
- Ulhe A, et al. Alpha-linolenic acid-mediated epigenetic reprogramming of cervical cancer cell lines. Epigenetics 20(1): 2451551, 2025. PubMed: 39895102
- Rani N, et al. Comparative In Vitro Anticancer Study of Cisplatin Drug with Green Synthesized ZnO Nanoparticles on Cervical Squamous Carcinoma (SiHa) Cell Lines. ACS Omega 8(16): 14509-14519, 2023. PubMed: 37125098
Herceptin Trastuzumab and Genentech are registered trademarks of Genentech, Inc.