- Drug Metabolism and Pharmacokinetic Studies
- Cytochrome P450 (CYP) Enzyme Activity: PHHs are widely used in drug metabolism studies because they express active cytochrome P450 enzymes, which are key to the metabolism of many drugs. Researchers use PHHs to examine which enzymatic pathways drugs go through in the liver and to predict drug clearance rates in humans.2
- Drug-Drug Interaction (DDI) Studies: PHHs can be used to evaluate how different drugs interact with each other when processed by the liver. These studies help in understanding competitive inhibition or induction of metabolic enzymes, which could affect drug safety and efficacy.1
- Phase I and Phase II Metabolism: PHHs are capable of conducting both Phase I (oxidation, reduction) and Phase II (conjugation) reactions, providing a complete in vitro system for predicting human drug metabolism and potential drug toxicity.3
- Toxicology and Safety Testing
- Hepatotoxicity Testing: PHHs are critical for predicting liver toxicity (hepatotoxicity) of pharmaceutical compounds. Because they retain liver-specific functions, they are a reliable model for detecting drug-induced liver injury (DILI), which is a major cause of drug withdrawal during clinical trials.4,5
- Chronic and Acute Toxicity: By maintaining cultures of PHHs over a prolonged period, researchers can assess both acute and chronic effects of drugs or chemicals on liver cells, making them ideal for studying long-term exposure risks.6
- Disease Modeling
- Liver Disease Models: PHHs are used to model liver diseases such as non-alcoholic fatty liver disease (NAFLD), non-alcoholic steatohepatitis (NASH), fibrosis, and cirrhosis. These models are crucial for studying the disease pathophysiology and for screening new therapeutic interventions.7
- Viral Hepatitis Research: PHHs are used to study viral infections, including hepatitis B (HBV) and hepatitis C (HCV), which target liver cells. These models are essential for understanding the lifecycle of these viruses and for testing antiviral drugs and vaccines.8
- Precision Medicine and Personalized Drug Testing
- Patient-Derived Hepatocytes: PHHs can be isolated from individual patients, allowing for personalized medicine approaches. By using hepatocytes from a specific patient, researchers can test how that person’s liver cells will respond to different drug treatments, helping to tailor treatments for optimal efficacy and minimal side effects.
- Genetic Variability Studies: PHHs derived from different individuals exhibit genetic and enzymatic variability, making them ideal for studying population-specific drug metabolism and toxicity. This helps in understanding inter-individual differences in drug responses.9
- Liver Transplantation and Regenerative Medicine
- Hepatocyte Transplantation: PHHs can be used in cell-based therapies for liver diseases. Transplantation of PHHs has been explored as a treatment for patients with acute liver failure or certain metabolic liver disorders, where hepatocytes perform essential liver functions temporarily or permanently.10
- Liver Regeneration Studies: Researchers use PHHs to understand the mechanisms involved in liver regeneration, which is key in developing regenerative medicine therapies for liver failure.11
- Bioartificial Liver Systems
- Extracorporeal Liver Support: PHHs are being explored for use in bioartificial liver devices that can temporarily perform liver functions for patients with liver failure. These devices use hepatocytes to detoxify blood and produce essential proteins and metabolites, giving patients more time to recover or wait for a liver transplant.12
- Metabolic Studies
- Lipid Metabolism and Steatosis: PHHs are used to study lipid metabolism and fatty acid accumulation in liver cells, which is particularly relevant in diseases like nonalcoholic fatty liver disease (NAFLD). Researchers can induce steatosis (fat accumulation) in PHHs to understand how metabolic disorders affect the liver and to screen potential treatments.13
- Glucose Metabolism: Since the liver plays a central role in glucose homeostasis, PHHs are ideal for studying the effects of drugs on glucose metabolism and for understanding how conditions like diabetes impact liver function.13
- Cholestasis Research
- Bile Acid Metabolism: PHHs are used to study bile acid synthesis and excretion, making them valuable for investigating cholestasis (a condition where bile flow is impaired), and testing drugs that may induce or alleviate this condition.14
- Gene Therapy Studies
- Viral Vector Testing: PHHs are a platform for evaluating the delivery and efficacy of viral vectors used in gene therapy. For example, researchers can use PHHs to assess the ability of viral vectors to deliver genes to the liver and to study gene expression or correction of genetic liver diseases.15
- CRISPR and Gene Editing: PHHs are used to explore gene-editing technologies like CRISPR/Cas9 in liver-targeted therapies. They provide a model for testing how gene editing can correct mutations or alter gene expression in the liver.16
- Endocrine and Hormonal Studies
- Hormonal Interactions: PHHs are also used to study how the liver interacts with hormones, such as insulin and glucagon. This is important in understanding diseases like diabetes and metabolic syndrome, where the liver's response to hormonal signals may be altered.17
Overall, PHHs are an indispensable tool for preclinical drug development, safety assessment, disease modeling, and regenerative medicine. They provide a highly relevant and functional system for studying liver biology and the effects of drugs and diseases on human liver function.
To support these critical focus areas, ATCC provides high-quality PHHs and media as well as detailed culture protocols for thawing and plating, media preparation, and maintenance and feeding. Our hepatocytes exhibit excellent viability and retain key liver functions, making them ideal for drug metabolism, toxicity studies, and liver disease research. Further, each batch undergoes rigorous testing to ensure consistency and reliability, including assessments of enzyme activity, protein expression, and metabolic function. Explore our models today and see how we can take your predictive drug development and toxicity testing to the next level.
Did you know?
ATCC primary human hepatocytes are sourced from multiple donors, reflecting the genetic variability found in the human population. This diversity allows for more comprehensive studies on how different genetic backgrounds can influence liver function and drug response.
Meet the author
Sopheap Sun, BS, MBA
Product Manager, Toxicology, ATCC
Sopheap Sun is an innovative leader in Biotechnology. He has over 22 years of experience in both cGMP manufacturing of Biologics and Product Management of Bioprocessing equipment, Cell Culture Media & Biologics, Cell & Gene Therapy products, and Cells. His Servant Leadership style of management allows him to develop high performing teams that develop and launch amazing products for the Life Sciences industry. Sopheap enjoys making our world better through Science and Technology.
Explore our featured resources
HepatoXcell™ Primary Human Hepatocytes
Discover how HepatoXcell™ provides a solution for your predictive drug development and toxicity testing.
More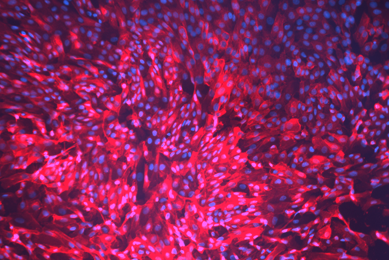
Toxicology
ATCC provides the tools you need to explore lung, skin, cardiovascular, gastro-enteric, liver, kidney, and neural toxicity. Our cells, media, and reagents help in toxicology research to identify responses to environmental toxins or to screen pharmaceutical compounds.
MoreViral Reference Materials
ATCC offers scientists viral reference materials for gene therapy research and as a benchmark for calibrating internal product-specific reference materials.
MoreReferences
- Zeilinger K, et al. Cell sources for in vitro human liver cell culture models. Exp Biol Med (Maywood) 241(15): 1684-1698, 2016. PubMed: 27385595
- Bachour-El Azzi P, et al. Expression and functional activity of cytochrome P450 enzymes in human hepatocytes with sustainable reproducibility for in vitro phenotyping studies. Adv Pharmacol 95: 285-305, 2022. PubMed: 35953158
- den Braver-Sewradj SP, et al. Inter-donor variability of phase I/phase II metabolism of three reference drugs in cryopreserved primary human hepatocytes in suspension and monolayer. Toxicol In Vitro 33: 71-79, 2016. PubMed: 26921663
- Godoy P, et al. Recent advances in 2D and 3D in vitro systems using primary hepatocytes, alternative hepatocyte sources and non-parenchymal liver cells and their use in investigating mechanisms of hepatotoxicity, cell signaling and ADME. Arch Toxicol 87(8): 1315-1530, 2013. PubMed: 23974980
- Ware BR, et al. Prediction of Drug-Induced Liver Injury in Micropatterned Co-cultures Containing iPSC-Derived Human Hepatocytes. Toxiol Sci 145(2): 252-262, 2015. PubMed: 25716675
- Hendriks DFG, et al. Mechanisms of Chronic Fialuridine Hepatotoxicity as Revealed in Primary Human Hepatocyte Spheroids. Toxicol Sci 171(2): 385-395, 2019. PubMed: 31505000
- Aasadollahea N, et al. Bioengineering liver microtissues for modeling non-alcoholic fatty liver disease. EXCLI J 22: 367-391, 2023. PubMed: 37223084
- Hwangbo S, et al. Analysis of host factor networks during hepatitis B virus infection in primary human hepatocytes. Virol J 21(1): 170, 2024. PubMed: 39090742
- Yang L, et al. Gene Expression Variability in Human Hepatic Drug Metabolizing Enzymes and Transporters. PLoS One 8(4): e60368, 2013. PubMed: 23637747
- Nulty J, et al. Human Hepatocyte Transplantation: Three Decades of Clinical Experience and Future Perspective. Stem Cells Transl Med 13(3): 204-218, 2024. PubMed: 38103170
- Liu Q, et al. Liver regeneration after injury: Mechanisms, cellular interactions and therapeutic innovations. Clin Transl Med 14(8): e1812, 2024. PubMed: 39152680
- Kumar A, et al. Extracorporeal Bioartificial Liver for Treating Acute Liver Diseases. J Extra Corpor Technol 43(4): 195-206, 2011. PubMed: 22416599
- Nagarajan SR, et al. Lipid and glucose metabolism in hepatocyte cell lines and primary mouse hepatocytes: a comprehensive resource for in vitro studies of hepatic metabolism. Am J Physiol Endocrinol Metab 316(4): E578-E589, 2019. PubMed: 30694691
- Boyer JL. Bio Formation and Secretion. Compr Physiol 3(3): 1035-1078, 2013. PubMed: 23897680
- Sands MS. AAV-mediated liver-directed gene therapy. Methods Mol Biol 807: 141-157, 2011. PubMed: 22034029
- Maestro S, et al. Novel vectors and approaches for gene therapy in liver diseases. JHEP Rep 3(4): 100300, 2021. PubMed: 34159305
- Klover PJ, Mooney RA. Hepatocytes: critical for glucose homeostasis. Int J Biochem Cell Biol 36(5): 753-758, 2004. PubMed: 15061128