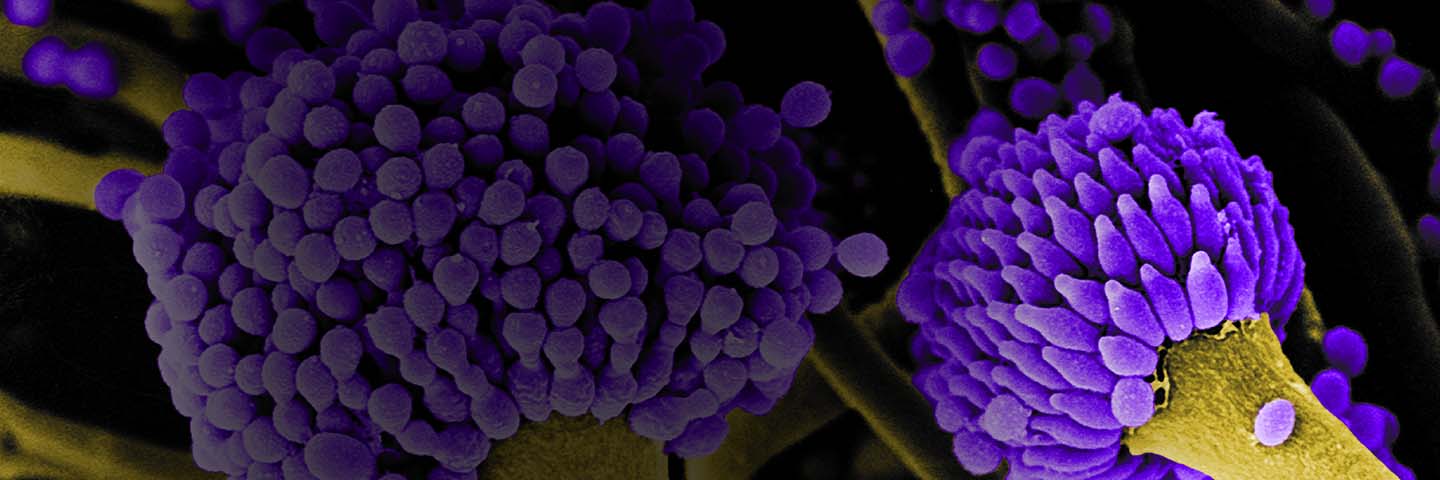
Over the past 20 years, Aspergillus fumigatus has become one of the most frequent causes of invasive fungal infection in immunocompromised individuals, resulting in a range of diseases collectively termed aspergillosis.1,2 Current therapies for aspergillosis include treatment with antifungal drugs such as Amphotericin B or Triazole medications (Voriconazole, Posaconazole, Itraconazole).3,4 Although the quality and efficacy of these antifungal therapies have significantly improved over the years, mortality due to invasive aspergillosis still remains high. This is further compounded by the growing number of antifungal drug-resistant strains, which has made the eradication of aspergillosis increasingly more difficult.
Download a PDF of this application note
Download NowTo aid in the analysis of novel antifungal medications, ATCC now offers a panel of A. fumigatus strains (ATCC MP-12) exhibiting various levels of sensitivity to common antifungal drugs. Each strain was examined for antifungal susceptibility using the Sensititre YeastOne YO9 colorimetric microdilution susceptibility test (TREK Diagnostic Systems, Cleveland, OH), according to the manufacturer’s instructions. A. fumigatus strains were prepared in YeastOne inoculum broth at an inoculum of 1.5-1.8 x 103 CFU/mL and were incubated at 35°C for 24 to 48 hours in the presence of Amphotericin B (0.12-8 µg/mL), Posaconazole (0.008-8 µg/mL), Voriconazole (0.008-8 µg/mL), or Itraconazole (0.015-16 µg/ mL). Fungal growth was evident as a change in the colorimetric growth indicator from blue (negative) to red (positive).
Each strain within the ATCC Aspergillus fumigatus Drug Testing Panel (ATCC MP-12) was found to be sensitive to Amphotericin B and displayed varying levels of sensitivity to the Triazole antifungal drugs. In particular, resistance to Posaconazole, Voriconazole, and Itraconazole was evident with strain FG1432 (ATCC MYA-3627), and increased sensitivity to these drugs was exhibited by strain NCMH 77 (ATCC 32820). Overall, this panel of strains exhibits varying levels of sensitivity to different antifungal drugs, illustrating that this unique set of strains is well suited for drug discovery, testing, and development, among other applications.
Table 1. ATCC Aspergillus fumigatus Drug Testing Panel (ATCC MP-12)
| ATCC number | Strain | Comments* | MIC (µg/mL) to Drugs** | |||
|---|---|---|---|---|---|---|
| Amphotericin B | Posaconazole | Voriconazole | Itraconazole | |||
| 1022 | QM 1981 | Type strain | 1 | 0.03 | 0.25 | 0.06 |
| 32820 | NCMH 77 | Albino variant | 2 | <0.008 | 0.06 | <0.015 |
| 90906 | 151 | T126C substitution | 2 | 0.015 | 0.25 | 0.06 |
| 96918 | SRRC 2006 | ICPA Reference | 1 | 0.06 | 0.5 | 0.12 |
| MYA-3626 | T33439 | CLSI M38-A2 | 1 | 0.03 | 0.25 | 0.12 |
| MYA-3627 | FG1432 | CLSI M38-A2 | 1 | 0.12 | 0.25 | 0.5 |
| MYA-4609 | Af293 | Genome Sequenced | 2 | 0.06 | 0.5 | 0.12 |
*T126C substitution refers to a base pair change in the ITS region of ATCC 90906 compared to the annotation of sequenced genome of ATCC MYA-4609; ICPA stands for International Committee on Penicillium and Aspergillus; and CLSI as Clinical Laboratory Science Institute.
**Minimal growth inhibitory concentration (µg/mL) is obtained by using TREK Diagnostic System’s YeastOne product. Each value in the table is average of two independent testings, recorded at the 48 hour incubation. The data, different from those obtained by using traditional broth dilution methods, are provided for information purpose only to show their relative sensitivity to each drug.
Download a PDF of this application note
Download Now
References
- Andriole V T. Infections with Aspergillus species. Clin Infect Dis. 1993;17:S481–S486.
- Groll A H, Shah P M, Mentzel C, Schneider M, Just-Nuebling G, Huebner K. Trends in the postmortem epidemiology of invasive fungal infections at a University Hospital. J Infect. 33:23–32, 1996.
- Herbrecht R, Denning DW, Patterson TF, Bennett JE, Greene RE, Oestmann JW, et al. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med. 347(6):408-415, 2002.
- Centers for Disease Control and Prevention. Treatment & Outcomes of Aspergillosis. http://www.cdc.gov/fungal/aspergillosis/treatment.html, 2012.