Why it’s important
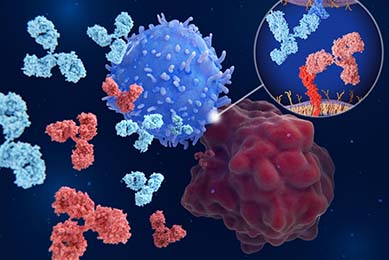
These novel therapeutics work by blocking the binding of immune checkpoint molecules on the immune cells to their ligands on the cancer cells. When this binding is blocked by immune checkpoint inhibitor molecules, the immune system is activated to kill the cancer cell.
Challenges
While this type of therapy is promising, developing new checkpoint inhibitor therapeutics can be challenging due to the lack of physiologically relevant models.
For instance, some of the current models used for the clinical development of these inhibitors are syngeneic mouse models and humanized mouse models.2 While these models provide valuable information in understanding immunological mechanisms and testing potential cancer immunotherapy drugs, they suffer from the inherent differences between the mouse immune system or human/mouse hybrid immune system and the human immune system.3
In vitro drug screens that use fully human ex vivo immuno-oncology assay models overcome the inter-species immune disparity. For example, co-culture assays of human T cells and human cancer cells can be used to observe the direct cytotoxic effects of T cells on cancer cells and evaluate inhibitor efficacy.4 The use of primary immune cells and patient-derived cells adds physiological relevance to the assay; however, these cells pose unique challenges such as natural donor variability issues and the experimental outcomes are often difficult to reproduce.5
Another alternative is the use of an artificial system comprising cancer cells engineered to overexpress immune checkpoint molecules that are co-cultured with non-cytotoxic T cells harboring a T cell activation signaling reporter gene. While this option solves the reproducibility problem, it loses physiological relevance due to the forced expression of the checkpoint molecules.6
What’s the solution?
To bridge the gap in checkpoint inhibitor therapeutic development, immuno-oncologists need access to physiologically relevant ex vivo reporter assay systems that incorporate cell lines that endogenously express high levels of immune checkpoint molecules. This type of reporter system would be more predictive of the in vivo situation while simultaneously allowing for the sensitive and qualitative assessment of signal transduction.
How we can help
At ATCC, we set out to help immuno-oncologists test their novel checkpoint inhibitor drug candidates by providing them tools to create a robust reporter assay system. Our scientists conducted comprehensive protein profiling of our portfolio of human cancer and immune cell lines for immune checkpoint molecules. Based on this proteomic data, we developed immune checkpoint reporter cancer cell lines that endogenously express high levels of immune checkpoint molecules.
The cancer reporter cells contain a gamma interferon activation site (GAS)-response element upstream of the luciferase gene. Additionally, we used single cell cloning to select cells exhibiting robust and stable expression. In a luciferase-based assay, these cells produce a bioluminescent signal in response to immune activation due to the presence of an immune checkpoint inhibitor.
The bioluminescence signal can be readily detected and quantified to evaluate the efficacy, potency, and pharmacodynamics of the inhibitor in a screening assay. These immune checkpoint reporter cancer cell lines yield exceptional in vitro and ex vivo assay sensitivity and reproducibility. Furthermore, the high endogenous expression of immune checkpoint molecules in these cell lines delivers physiological relevance to the checkpoint assay.
Did you know?
At ATCC, we set out to help immuno-oncologists test their novel checkpoint inhibitor drug candidates by providing them tools to create a robust reporter assay system.
Hyeyoun Chang, PhD
Scientist, ATCC
Hyeyoun Chang, PhD, is a Scientist in the Immuno-oncology group of the R&D department at ATCC. She has extensive experience in the fields of biomedical engineering and cancer biology that focuses on drug delivery, intracellular signaling, and gene therapy. Prior to joining ATCC, Dr. Chang received her PhD in biomedical engineering from Korea University of Science and Technology and completed her postdoctoral training at Dana-Farber Cancer Institute/ Harvard Medical School.
Brian Shapiro, PhD
Marketing Segment Manager, Oncology, ATCC
Brian A Shapiro, PhD, works to communicate the scientific breakthroughs of ATCC’s product development laboratories to the biomedical research community. Brian is the Executive Producer of ATCC's Podcast, Behind the Biology. Previously, he worked at Virginia Commonwealth University, where he investigated the role of pre-mRNA splicing in the multi-drug resistance of lung cancer. Dr. Shapiro attended the Medical College of Georgia, where his research focused on adrenal physiology as well as diseases of the epidermis.
Hai-y Le, MA
Digital Content Specialist
Hai-y is a Digital Content Specialist at ATCC who loves collaborating with her colleagues and communicating essential information to the public to galvanize better health and science outcomes. She previously worked at the Public Health Department of Santa Clara County, California, wrote for The San Francisco Chronicle, and coordinated editorial content at The Atlantic Council think tank in Washington, D.C. She has an MA in Communication and BA from Stanford University.
Checkpoint Luciferase Reporter Cells
ATCC created tumor and immune cell lines with high endogenous expression of checkpoint inhibitory and co-stimulatory expression levels. Learn how you can integrate these reporter cells in the development of new checkpoint inhibitors for immuno-oncology drug discovery.
MoreReferences
- Korman AJ, et al. The foundations of immune checkpoint blockade and the ipilimumab approval decennial. Nat Rev Drug Discov 21: 509-528, 2022. PubMed: 34937915
- Kubli SP, et al. Beyond immune checkpoint blockade: emerging immunological strategies. Nat Rev Drug Discov 20: 899-919, 2021. PubMed: 33686237
- Olson B, et al. Mouse models for cancer immunotherapy research. Cancer Discov 8: 1358-1365, 2018. PubMed: 30309862
- Dijkstra KK, et al. Generation of Tumor-Reactive T Cells by Co-culture of Peripheral Blood Lymphocytes and Tumor Organoids. Cell 174: 1586-1598 e1512, 2018 PubMed: 30100188
- Versteven M, et al. A versatile T cell-based assay to assess therapeutic antigen-specific PD-1-targeted approaches. Oncotarget 9: 27797-27808, 2018. PubMed: 29963238
- Ribas A, Wolchok JD. Cancer immunotherapy using checkpoint blockade. Science (359): 1350-1355, 2018. PubMed: 29567705